BASAL THUMB ARTHRITIS
- Matt Giles
- Dec 26, 2021
- 6 min read
Updated: Jul 21
WHAT IS BASAL THUMB ARTHRITIS?
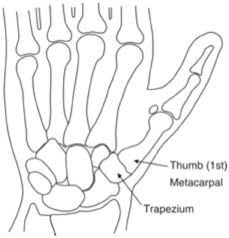
What Causes Basal Thumb Arthritis? The thumb is the most important digit in the hand. Without adequate and pain free movement of the thumb, the function of the hand is significantly reduced. The bone at the base of the thumb (the metacarpal) forms a joint with one of the wrist bones (the trapezium). See Fig. 1. This forms the basal thumb joint. Smooth, slippery cartilage normally covers the ends of the bones at the joint and acts to reduce the friction at the joint to allow easy movement and also acts as a shock-absorbing layer. Wear and tear on the cartilage that covers the ends of the bones causes the cartilage to wear away and the raw bone ends to rub on each other. This causes pain and deformity of the joint so that the base of the metacarpal sticks out to the side causing a lump and the span of the hand is reduced (see Fig. 2).
FIG.1Normal thumb base
FIG.2Arthritic thumb base
Diagnosis of Basal Thumb Arthritis Your Surgeon will discuss your symptoms with you and will examine your thumb to see exactly where your pain is located. There are several joints in the hand and wrist, which are very close together and may give similar symptoms. X-rays will be taken, some in special positions to highlight the joint.
Treatment of basal thumb arthritis Injection. A small volume of steroid and local anaesthetic may be injected into the joint. This does not cure the arthritis but it can help to relieve the pain for a variable time (weeks to months). It may also be used in diagnosis to check that a specific joint is the cause of pain. Injection may be repeated up to 3 times. The pain in the joint often flares up for 48 hours after the injection and then settles. There is a very small chance of infection and occasionally the skin over the injection site becomes a little paler.
Splints. Various splints may be tried, usually to help with pain on using the hand. They do not need to be worn all of the time but only when the thumb is sore or when doing activities that cause pain. A specific referral from your GP may be required for splinting. Surgery. This may be done as a day case operation. That means you will normally only have to be in the hospital for half a day and not over night. Do not drive to the hospital yourself. You will need a responsible adult to pick you up after your surgery. Sometimes, people are admitted to the hospital over night. This is usually planned before the surgery and may be for medical or social reasons. The surgery may be carried out under a general anaesthetic with you asleep or a regional anaesthetic with only the arm “frozen”.
You will be given a gown to wear on the ward before the operation is carried out. It is recommended that you wash your hands with soap and water before the operation. Make sure your nails are clean. One of several types of operation may be performed depending on symptoms, age, level of function and patient requirements.

FIG.3Trapeziectomy
Trapeziectomy. This is the commonest procedure and involves removing the trapezium bone entirely. This removes one of the rough and painful joint surfaces, stopping the raw bone ends from rubbing together and helps pain (Fig. 3). A stabilisation procedure is performed as well either using a tendon or membranes from around the joint. Depending on your surgeon, a wire may be placed temporarily for a few weeks to hold the thumb in position whilst it heals. It is then removed in clinicThe thumb and wrist are placed in a plaster cast for 4 weeks. The fingers are left free and should be moved, as should the tip of the thumb. After this time the wrist and thumb may be placed in a plastic splint for a further 2 weeks whilst physiotherapy is started to help thumb movement. After 6 weeks, the hand is left free to move and it may take up to 6 months for it to completely settle down after the surgery.
Joint replacement. This operation is less commonly done and usually for younger people who are still working. The post-operative treatment is similar to trapeziectomy. The aim is to give a slightly stronger thumb joint than for trapeziectomy but at the risk of a further operation in the future if the artificial joint replacement wears out, fails or dislocates. In these circumstances, the replacement may be revised to a trapeziectomy. A joint replacement cannot be carried out if the basal thumb joint is very deformed or if the bone is thin.
Denervation. Occasionally, a procedure is carried out to cut the nerves to the basal thumb joint. This does not stop the joint moving and does not treat the arthritis but can help the pain, usually for a couple of years. The feeling of the skin is not affected. Occasionally the pain is not helped sufficiently. The benefit of this procedure is that it does not require as much time off work and preserves strength and movement but is the least likely to give long-term pin relief.
Arthrodesis. This is a fusion of the joint at the base of the thumb. It removes 70% of movement of the base of the thumb and the fusion may not knit in 10% of cases. However, it gives a very strong thumb, which may be useful in patients who do manual work or if the base of the thumb is very unstable.
Metacarpophalangeal joint procedures. If the thumb tends to bend back on itself at the joint above the thumb base (the last but one joint of the thumb) then a procedure to stop this may be advised. This may be called a volar plate advancement, a sesamoid arthrodesis or other procedure. It is done at the same time as the basal thumb surgery and does not usually change the postoperative treatment much.
After the Operation You will find that there is a partial plaster cast on your wrist and thumb unless you have had a denervation, when only soft bandages are applied. Keep your hand elevated at head level to reduce swelling. The plaster cast will be removed and changed after 2 weeks when the wound is checked. It is removed at 4 weeks to allow physiotherapy to start. You will have a plastic splint made to support the thumb until 6 weeks post op. When the plaster cast is removed, you will be asked to start massaging the scar with a moisturiser e.g. E45.
You may get back to driving after 6-7 weeks and can consider going back to light work 7-8 weeks after surgery.
Risks of Surgery In the vast majority of cases surgery is successful but this may be a technically difficult operation and there are some possible complications of surgery that you should know about.
Stiffness and swelling of the fingers is common. Keeping the hand well elevated and early movement tends to limit this. Rarely, severe swelling, stiffness and pain occurs which does not quickly settle. This is called reflex sympathetic dystrophy and requires protracted therapy.
The majority of patients get good or excellent pain relief but occasionally a little aching or intermittent twinges of discomfort remain but these are much less severe than the preoperative pain. The hand may take up to 6 months to completely settle after the surgery.
Infection is uncommon but does occasionally occur. It usually settles well with antibiotics but occasionally requires reoperation.
There are small arteries and nerves around the base of the thumb that are vulnerable to injury whilst the incision is being made. Occasionally the artery can cause some bleeding. Cutting a small nerve may cause some loss of feeling on the back of the thumb. Even when the arteries and nerves are not damaged a proportion of patients have slightly less feeling than before over the back of the thumb. This settles with time. Rarely, the base of the thumb may become unstable and too “wobbly” after surgery. This causes pain and loss of strength and often requires reoperation.
One-Handed Living Do not forget that you will not be able to use the hand that has been operated on fully for a short while after surgery. Make life easy for yourself at home by planning ahead, particularly if you are alone at home or if you will be alone at home for long periods in the day.
Get enough shopping in to last for a week or two after your surgery, as you will not be able to drive. Loosen the tight caps of jars (but don’t forget the contents will go off more quickly). Ready-meals might be useful for a few days after surgery or do some cooking before and freeze it. Wear slip-on shoes so you don’t have to tie laces etc.

Comments